Two recent papers have provided strong evidence that the brain's endocannabinoid system is dysfunctional in Huntington's Disease, paving the way to possible new treatments. Huntington's Disease is a genetic neurological disorder. Symptoms generally appear around age 40, and progress gradually from subtle movement abnormalities to dementia and complete loss of motor control. It's incurable, although medication can mask some of the symptoms. Singer Woodie Guthrie is perhaps the disease's best known victim: he ended his days in a mental institution.
Huntington's Disease is a genetic neurological disorder. Symptoms generally appear around age 40, and progress gradually from subtle movement abnormalities to dementia and complete loss of motor control. It's incurable, although medication can mask some of the symptoms. Singer Woodie Guthrie is perhaps the disease's best known victim: he ended his days in a mental institution.
The biology of Huntington's is only partially understood. It's caused by mutations in the huntingtin gene, which lead to the build-up of damaging proteins in brain cells, especially in the striatum. But exactly how this produces symptoms is unclear.
The two new papers show that cannabinoids play an important role. First off, Van Laere et al used PET imaging to measure levels of CB1 receptors in the brain of patients in various stages of Huntington's. CB1 is the main cannabinoid receptor in the brain; it responds to natural endocannabinoid neurotransmitters, and also to THC, the active ingredient in marijuana.
They found serious reductions in all areas of the brain compared to healthy people, and interestingly, the loss of CB1 receptors occurred early in the course of the disease:
They found that Huntington's mice who also had a mutation eliminating the CB1 receptor suffered more severe symptoms, which appeared earlier, and progressed faster. This suggests that CB1 plays a neuroprotective role, which is consistent with lots of earlier studies in other disorders.
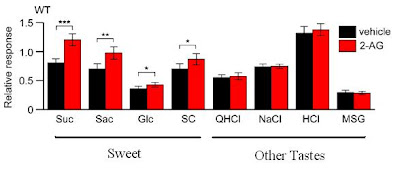
If so, drugs that activate CB1 - like THC - might be able to slow down the progression of the disease, and indeed it did: Huntington's mice given THC injections stayed healthier for longer, although they eventually succumbed to the disease. Further experiments showed that mutant huntingtin switches off expression of the CB1 receptor gene, explaining the loss of CB1.
This graph shows performance on the RotaRod test of co-ordination: mice with Huntington's (R6/2) got worse and worse starting at 6 weeks of age (white bars), but THC slowed down the decline (black bars). The story was similar for other symptoms, and for the neural damage seen in the disease.
Altogether, these results support the notion that downregulation of type 1 cannabinoid receptors is a key pathogenic event in Huntington’s disease, and suggest that activation of these receptors in patients with Huntington’s disease may attenuate disease progression.Now, this doesn't mean people with Huntington's should be heading out to buy Bob Marley posters and bongs just yet. For one thing, Huntington's disease often causes psychiatric symptoms, including depression and psychosis. Cannabis use has been linked to psychosis fairly convincingly, so marijuana might make those symptoms worse.
Still, it's very promising. In particular, it will be interesting to try out next-generation endocannabinoid boosting drugs, such as FAAH inhibitors, which block the breakdown of anandamide, one of the most important endocannabinoids.
In animals FAAH inhibitors have pain relieving, anti-anxiety, and other beneficial effects, but they don't cause the same behavioural disruptions that THC does. This suggests that they wouldn't get people high, either, but there's no published data on what they do in humans yet...
Blázquez C, et al. (2010). Loss of striatal type 1 cannabinoid receptors is a key pathogenic factor in Huntington's disease. Brain : a journal of neurology PMID: 20929960


 05.10
05.10
 wsn
wsn
 Posted in
Posted in